Dry Eye Causes and Patient Symptoms / Complaints
Dry eye disease (DED) is an ocular condition that afflicts many people in some form. The TFOS DEWS II Epidemiology Report1 estimates the prevalence of DED to range from 5 to 50%. Their analysis confirmed that prevalence increases with age, women have a higher prevalence than men, although differences become significant only with age.
The report goes on to state “The economic burden and impact of DED on vision, quality of life, work productivity, psychological and physical impact of pain, are considerable, particularly costs due to reduced work productivity.”
Let’s take a more detailed look at this condition and how it may impact contact lens wear.
The front surface of the eye is bathed in fluid and is known as the tear film and consists of three layers: lipid (oily), aqueous (watery), and mucin (mucous) layer. Each has a specific role in keeping the surface of the eye wet. (Figure 1)
Any time these layers are out of balance (tear dysfunction) with each other the effective result is a “dry” eye.
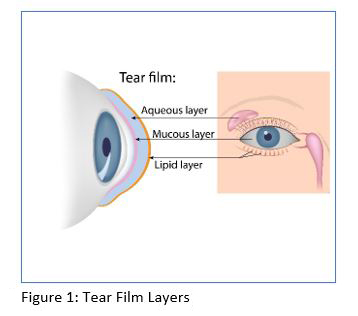
This dryness could be from a decrease in tear production or increase in evaporation. For instance, if the lacrimal glands are not producing enough tears it results in aqueous insufficiency.
A slight decrease in tear production could simply be a part of the aging process. Ocular allergies can play a role here. In more extreme situations, severe dry eye could be associated with medical disorders with rheumatoid arthritis and thyroid conditions being illustrations of this, as well. Medications such as antihistamines and decongestants may also impact tear production.
The oily nature of the lipid layer aids in decreasing tear evaporation. This layer is secreted by the meibomian glands and if these glands become clogged there may not secrete enough “meibum.” This is often referred to as meibomian gland dysfunction or MGD.
Other causes of increased tear evaporation may be poor secretion by the conjunctival goblet cells of mucin. The mucin layer’s function is to “hold” the aqueous layer on the eye for as long as possible between the eyelid blink cycle.
Other evaporated causes are poor blinking (often related to excessive computer use or near visual tasks), eyelid abnormalities such as ectropion and entropion, chemical preservatives in eye drops or contact lens solutions and allergies.
So, how is contact lens wear effected by “dry eyes?” The answer to this is both positively and negatively depending on the situation.
First, soft lens wearers that suffer from dry eye often have difficult achieving prolonged wear. Soft contact lenses have fluid contents of 38% to 75% and when worn they function like a sponge and soak up as much of the tear layer as possible to remain hydrated. In fact, many SCL manufacturers use special materials and/or surface treatments in an attempt keep the lenses wet during wear. SCLs that dry out often become “tight” causing increased awareness, redness and sometimes discomfort. This is likely the primary reason for SCL dropout today.
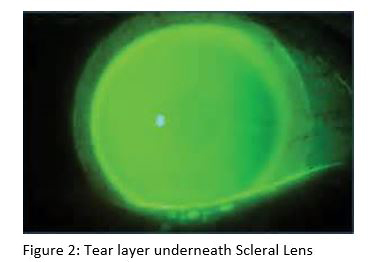
Alternatively, Scleral GP lenses can increase patient comfort and wear time. Since they have no fluid content, they don’t need tears to maintain their form. Most importantly, the fluid layer formed between the back surface of the lens and the eye (Figure 2) can keep the cornea bathed in tears throughout the wearing time.
References
1 Fiona Stapleton, Monica Alves, et al; TFOS DEWS II Epidemiology Report; http://dx.doi.org/10.1016/j.jtos.2017.05.003